Afr. J. Parasitol. Mycol. Entomol. , 3(1), 4; doi:10.35995/ajpme03010004
Article
Knowledge and Practices of Private Nurseries Regarding the Management of Malaria in 2022 in Abidjan, Côte d’Ivoire
1
Laboratory of Parasitology, Mycology, Animal Biology and Zoology, Department of Pharmacy, Felix Houphouët-Boigny University, P.O. Box V 34, Abidjan, Cote d’Ivoire; sebastienmiezan@yahoo.fr (M.A.J.S.); akouaval@yahoo.fr (B.-T.A.V.); vangahenriette@yahoo.fr (V.-B.A.H.); angorakpongbo2005@yahoo.fr (A.K.E.); kikipcm@yahoo.fr (K.-B.P.C.M.); abykonate@yahoo.fr (K.-T.A.); kasful2000@yahoo.fr (K.K.F.); vincentdjohan1@yahoo.fr (D.V.); yavowilliam@yahoo.fr (Y.W.); rvmenan@yahoo.fr (M.E.I.H.)
2
Parasitology and Mycology Unit, Center for Diagnosis and Research on AIDS and Other Infectious Diseases (CeDReS), University Hospital of Treichville, P.O. Box V 13, Abidjan, Cote d’Ivoire; alaingnamian@gmail.com
*
Corresponding author: dignanyo@yahoo.fr; Tel.: +225-21-25-84-59; Fax: +225-21-24-92-06
How to cite: Massafoma, K.E.G.; Sebastien, M.A.J.; Valérie, B.-T.A.; Henriette, V.-B.A.; Etienne, A.K.; Marie, K.-B.P.C.; Alain, G.N.K.; Abibatou, K.-T.; Fulgence, K.K.; Vincent, D.; et al. Knowledge and Practices of Private Nursery Regarding the Management of Malaria in 2022, Abidjan, Côte d’Ivoire. Afr. J. Parasitol. Mycol. Entomol. 2025, 3(1): 4; doi:10.35995/ajpme03010004.
Received: 21 February 2025 / Accepted: 4 July 2025 / Published: 17 September 2025
Abstract
: To tackle the impact of malaria in countries where it is prevalent, it is crucial for important parties to participate in control initiatives. However, in Côte d’Ivoire, the National Malaria Control Programme (NMCP) has excluded the private sector nursery activities, which play an important role in malaria surveillance. Therefore, a study was conducted in Abidjan to assess the knowledge and practices of private nurseries in regard to the National Malaria Treatment Policy. A cross-sectional survey was carried out from January to June 2012. The survey targeted all private nursery health professionals who treated patients with suspected malaria cases in the Abidjan District of Côte d’Ivoire. A questionnaire was administered to the practitioners to evaluate their knowledge and practices regarding malaria and the National Malaria Treatment Policy. We interviewed 161 practitioners who worked at 200 private nurseries that were visited. Among them, 96 (55.1%) were nurses and 46 (28.6%) were orderlies. The remaining practitioners were made up of physicians (9.3%) and midwives (2.5%) who were hired. The study found a significant relationship between the professional status of the practitioners and their knowledge of new NMCP guidelines or activities. The majority of the practitioners (89/161; 55.3%) provided antimalarial treatment using artemisinin-based combination therapies (ACTs) in the event of a negative rapid diagnostic test (RDT) result. This practice was observed across all professional status categories, with orderlies (58.7%), nurses (58.4%), and midwives (50%) being more inclined to offer this treatment. It is necessary to implement targeted interventions to enhance health workers’ practice.
Keywords:
malaria; NMCP guidelines; case management; compliance; “test and treat”; Côte d’Ivoire1. Introduction
Malaria is a significant public health concern that affects tropical regions of America, Africa, the Eastern Mediterranean, Southeast Asia, and the Western Pacific. In 2022, there were approximately 249 million reported cases and 608,000 deaths [1]. Globally, twenty-nine countries, including Côte d’Ivoire, were the home of 96% of malaria cases and deaths. In 2022 and 2021, the malaria incidence rate in Côte d’Ivoire was 1534 per 1000 and 1271 per 1000 in the general population and 1534 per 1000 and 1068 per 1000 in children under five [1,2].
The global shift from presumptive fever treatment to the 2010 “test and treat” policy was a significant milestone in the history of malaria case management [3,4]. This policy recommended parasitological testing of all suspected malaria cases and targeted antimalarial treatment for only confirmed cases. There is an urgent need for health workers to follow the guidelines for the proper management of malaria cases since it is a determinant in ensuring the best outcomes [5].
Several studies conducted across Africa on outpatient malaria case management revealed that health workers do not always comply with testing recommendations [6,7,8], use non-recommended antimalarials for confirmed cases [9], provide irrational antimalarial treatments for test-negative patients [10], and miss opportunities to administer prompt antimalarial treatment at health facilities [11,12].
The public and private sectors must be actively involved in applying new treatment guidelines and recommendations practically. However, the participation of the private sector in the actions and campaigns organized by the National Malaria Treatment Policy (NMTP) (known locally as the Programme National de Lutte contre le Paludisme, PNLP) is almost nonexistent [13,14]. This lack of involvement is particularly alarming given the indispensable role those private nurseries, commonly known as “neighbourhood infirmaries”, play in the healthcare system of Côte d’Ivoire. The proximity of these facilities to the population makes them one of the primary sources of health care for many households, especially the most vulnerable. Importantly, the thick drop method, rapid diagnostic test, and treatment are free of charge in public health centres, which is not the case in the private sector. However, in Côte d’Ivoire, very few studies have reported on the possible impact of excluding private infirmaries from the activities of the NMTP. Therefore, their knowledge and adherence to malaria management guidelines are paramount.
2. Materials and Methods
2.1. Study Area
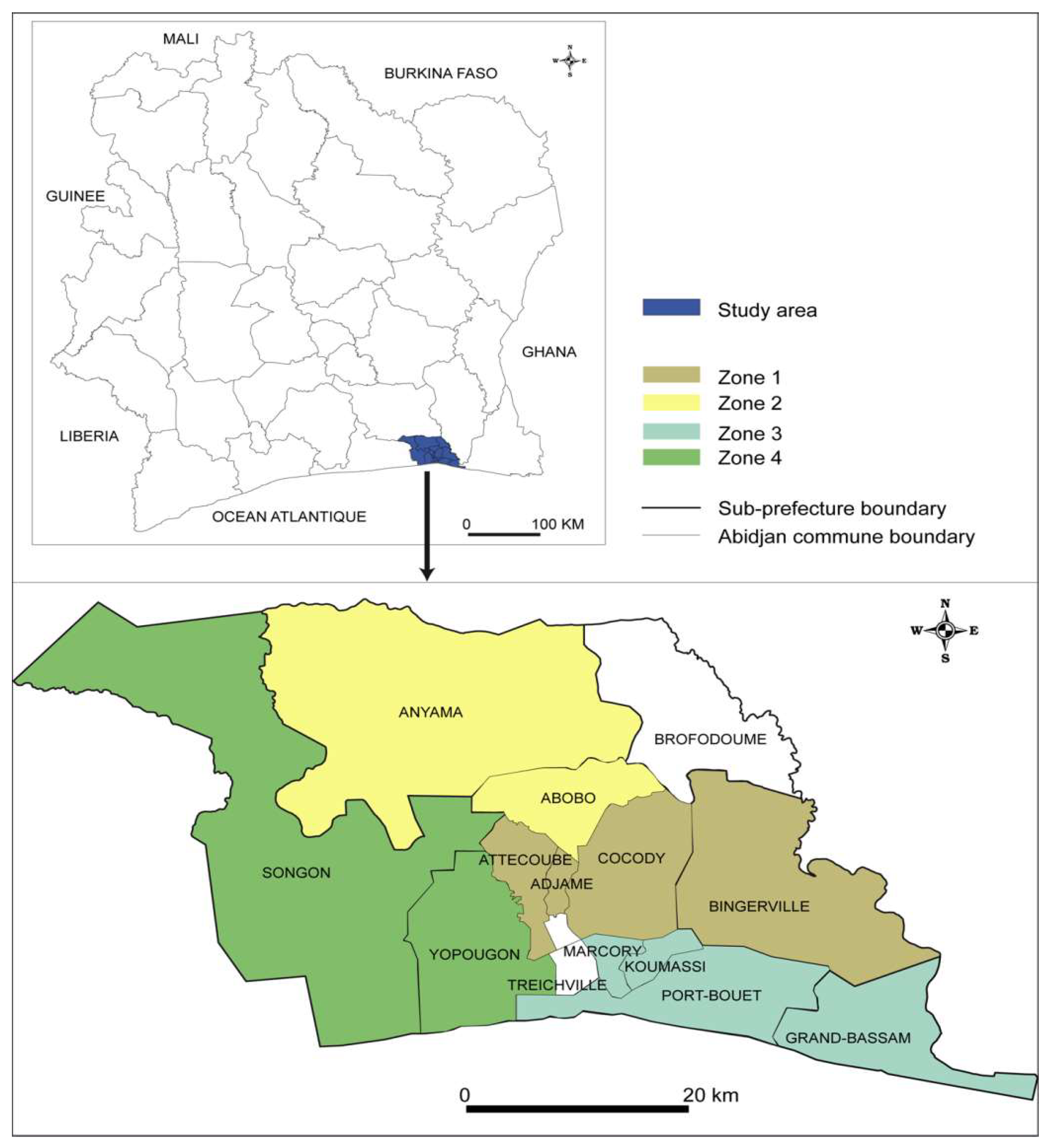
From January to June 2022, a survey was carried out that gathered information from different groups of people at the same time in a private nursery in Abidjan, the economic capital of Côte d’Ivoire (Ivory Coast). Abidjan is the country’s financial capital. It is located on the coast and experiences a humid, equatorial-type climate with two rainy seasons (April to July and October to November) and two dry seasons (December to March and August to September). The range of temperature is between 25 °C and 30 °C, while the relative humidity fluctuates between 80% and 90%. Anopheles gambiae and Anopheles funestus are the most prevalent vectors for malaria transmission in this area. The majority of malaria infections, comprising over 95%, are caused by Plasmodium falciparum [15].
Côte d’Ivoire is divided into 33 health regional directions (HRDs). The District of Abidjan includes two of the 33 HRDs. The Abidjan 1 HRD includes six health district directions (HDDs), one teaching hospital, five general hospitals, and one hundred and seven first-contact health facilities. The Abidjan 2 HRD includes six health district directions (HDDs), three teaching hospitals, nine general hospitals, and three hundred and eleven first-contact health facilities.
2.2. Study Procedures
The Abidjan 1 health regional direction includes six DSs, one teaching hospital, five general hospitals, and one hundred and seven first-contact health facilities (ESPCs). The Abidjan 2 regional health directorate has six DSs, three teaching hospitals, nine HGs, and three hundred and eleven ESPCs.
In 2022, the Department of Health Care Facilities and Professions (HCFP) provided a list of all the private nurseries in the District of Abidjan. This list included 272 infirmaries grouped into four (4) zones:
- Zone 1: Adjamé–Cocody–Bingerville (55)
- Zone 2: Abobo–Anyama (42)
- Zone 3: Marcory, Koumassi, and Port-Bouët (73)
- Zone 4: Yopougon–Songon (102)
At the time of the present study, no previous studies have been carried out to show the proportion of the contribution of nurseries to malaria management in Abidjan.
We implemented the study in all of these communes except Songon and Grand-Bassam. Despite the HCFP’s authorizations for the survey, officials in both communes refused. We excluded the Plateau commune because, according to HCFP data, it is not home to any infirmaries (Figure 1).
Figure 1.
Map of Abidjan District including study areas.
Armed with the survey authorization issued by the HCFP, we made an appointment with the head of the health facility to obtain his agreement to carry out the survey. Our team used a particular questionnaire for each practitioner.
At the beginning of the study, we enrolled private nurseries that met the recruitment standard.
Practitioners with a minimum of five years of experience in their role, with or without specialized training, were included after obtaining free and informed consent. On-site, they interviewed only one practitioner by private service whenever the selected candidate met the criteria.
The data collection material was a specific standardized questionnaire, pre-tested before the beginning of the study. It was administered to different practitioners to collect data on their levels of knowledge and other practices in managing malaria.
Practitioners were surveyed about their practices, knowledge of malaria, and adherence to the National Malaria Treatment Guidelines (NMCP). The questionnaire included questions about their sociodemographic characteristics (gender, level of education, and number of years of practice), knowledge of malaria (epidemiology, clinical signs, biological tests, and treatment), and the recommendations given by the NMCP.
All participants in this study were informed of the confidentiality of their answers during the interview, their anonymity, and their right to withdraw at any time.
In 2018, the Côte d’Ivoire NMTP recommended ASAQ, AL, or DHA PQ as the first-line treatment for uncomplicated malaria in anyone except pregnant women. Oral quinine (QN) is recommended as a second-line treatment if ASAQ, AL, and DHA PQ are ineffective or unavailable.
Intravenous Artesunate is recommended for severe malaria. Complete ACT therapy should be given orally after the patient regains consciousness. If Artesunate is unavailable, quinine or artemether should be administered [16].
Our study included healthcare providers practising in a private nursery located geographically in our study area who provided consultations and prescriptions and agreed to participate in the survey.
2.3. Statistical Analysis
The software EPI Info 6.04 (CDC, Atlanta, GA, USA) was utilized to analyze the collected data. Parameters such as proportions, mean, standard deviation, minimum, and maximum were used to describe the study population. Percentages were determined by considering the total number of respondents per question. Common themes were derived from responses to open-ended questions. To investigate the statistical association between the two variables, either Pearson’s chi-square test or Fisher’s exact test was utilized. Values of p ˂ 0.05 are considered statistically significant. For theoretical group sizes less than or equal to 5, Fisher’s exact test was used.
2.4. Ethical Considerations
The survey was based solely on questioning, which posed no danger to the interviewees. On the contrary, it enabled a fruitful exchange of information between the private nursery and the interviewer. Participation in the survey was free and without constraint, and all interviewees could voluntarily stop their participation at any time during the study.
3. Results
3.1. Socio-Professional Characteristic
Out of a total of 272 private nurseries, investigators located 200 private nurseries based on the geographical address communicated by the HCFP. Of the 200 private nurseries visited, 161 agreed to participate in our survey, who were usually the people in charge of the structure.
Therefore, our study involved 161 prescribers, most of whom were male (55.9%). Nurses accounted for 55.1% (96) of all prescribers, compared with 46 orderlies (28.6%). Physicians (9.3%) and midwives (2.5%) were poorly represented (Table 1). The role of orderlies is to look after the hygiene and physical and moral comfort of patients, under the responsibility of the nurse. However, in the infirmaries, they consult patients and issue medical prescriptions.
Table 1.
Practitioner demographics according to study area.
| Cities | Area 1 | Area 2 | Area 3 | Area 4 | Total |
|---|---|---|---|---|---|
| Attécoubé–Adjamé–Cocody–Bingerville (55) | Abobo–Anyama (42) | Marcory–Koumassi–Port-Bouët (62) | Yopougon–Songon (102) | ||
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Sex | |||||
| Male | 22 (57.9) | 17 (56.7) | 17 (45.9) | 34 (60.7) | 90 (55.9) |
| Female | 16 (42.1) | 13 (43.3) | 20 (54.1) | 22 (39.3) | 71 (44.1) |
| Professional status | |||||
| Nurse | 21 (55.3) | 18 (60) | 28 (75.7) | 29 (51.8) | 96 (59.6) |
| Orderly | 14 (36.8) | 5 (16.7) | 9 (24.3) | 18 (32.1) | 46 (28.6) |
| Midwife | 1 (2.6) | 2 (6.6) | 0 | 1 (1.8) | 4 (2.5) |
| Doctor | 2 (5.3) | 5 (16.7) | 0 | 8 (14.3) | 15 (9.3) |
| Years of experience | |||||
| <5 | 15 (39.5) | 9 (37.5) | 5 (13.5) | 21 (37.5) | 50 (31.05) |
| 6–10 | 7 (18.4) | 15 (50.0) | 6 (16.2) | 15 (26.8) | 32 (19.9) |
| 11–20 | 4 (10.5) | 4 (13.3) | 8 (21.6) | 8 (14.3) | 26 (16.1) |
| 15–20 | 5 (13.2) | 5 (16.7) | 7 (18.9) | 6 (10.7) | 23 (14.3) |
| >20 | 7 (18.4) | 6 (20.0) | 11 (29.7) | 6 (10.7) | 30 (18.6) |
| Total | 38 (100.0) | 30 (100.0) | 37 (100.0) | 56 (100.0) | 161 (100.0) |
3.2. General Knowledge Regarding Malaria
Regarding malaria transmission, 100% of practitioners knew that a mosquito bite transmits malaria, and 99.3% (140/141) answered that Plasmodium is the microorganism responsible for the disease.
The clinical signs of uncomplicated malaria were well-known to the participants. Almost all the practitioners mentioned fever (100%), followed by headache (99.3%) and body aches (99.8%). Convulsions, anemia, prostration, and loss of consciousness were mentioned by 99.3%, 97.8%, 95.7%, and 95.03% of practitioners, respectively, when asked about complicated malaria signs and symptoms. Concerning the biological diagnosis of malaria, the first test mentioned by practitioners was the rapid diagnostic test (92.9%), followed by the thick drop method (7.1%) (Table 2). Table 2 shows this in more detail.
Table 2.
Knowledge about malaria and its signs, symptoms, and diagnosis.
| Variables | n | % |
|---|---|---|
| Malaria transmission | ||
| Bite of the female anopheles | 141 | 100 |
| Microorganism responsible for the disease | ||
| Plasmodium | 140 | 99.3 |
| Other | 1 | 0.7 |
| Major clinical signs | ||
| Fever | 141 | 100 |
| Headache | 140 | 99.3 |
| Body aches | 138 | 99.8 |
| Signs and symptoms of severe malaria | ||
| Convulsions | 140 | 99.3 |
| Anemia | 138 | 97.8 |
| Prostration | 135 | 95.7 |
| Loss of consciousness | 134 | 95.03 |
| Malaria diagnosis method you use before treatment | ||
| Rapid diagnostic test (RDT) | 131 | 92.9 |
| Microscopy | 10 | 7.1 |
3.3. The National Malaria Treatment Guidelines (NMCP)
Most of the practitioners at the health centres (87.67%) said they knew the National Malaria Treatment Guidelines (Table 3), while nurses (72.9%) and orderlies (84.87%) said they did not know it (66.7%). A statistically significant relationship between knowledge of the new NMCP guidelines and professional status (p = 0.00027) was observed (Table 3). Most practitioners who were aware of the guidelines stated that they had heard about it through a colleague (72.8%), followed by medical visitors (27.2%).
Table 3.
Knowledge of duration and dosage of antimalarial recommended as 1st-line treatment for uncomplicated malaria in children and adults by professional status of healthcare providers according to their professional status.
Table 3.
Knowledge of duration and dosage of antimalarial recommended as 1st-line treatment for uncomplicated malaria in children and adults by professional status of healthcare providers according to their professional status.
| Professional Status | Knowledge of New NMCP Guidelines | |||||
|---|---|---|---|---|---|---|
| Yes | No | p | ||||
| Total | n | % | n | % | ||
| Doctor | 15 | 10 | 66.7 | 5 | 33.3 | |
| Nurse | 96 | 26 | 27.1 | 70 | 72.9 | 0.00027 |
| Midwife | 4 | 3 | 75 | 1 | 25 | |
| Orderly | 46 | 7 | 15.2 | 39 | 84.8 | |
| Total | 161 | 141 | 87.6 | 20 | 12.4 | |
| Knowledge of anNMCPactivity | ||||||
| Yes | No | p | ||||
| Total | n | % | n | % | ||
| Doctor | 15 | 15 | 100 | 0 | 0 | |
| Nurse | 96 | 56 | 58.3 | 40 | 41.7 | 0.0026 |
| Midwife | 4 | 3 | 75 | 1 | 25 | |
| Orderly | 46 | 21 | 45.7 | 25 | 54.3 | |
| Total | 161 | 95 | 37.9 | 66 | 62.1 | |
| Antimalarial Drugs Usually Prescribed to Children | ||||||
| Correct Dosage | Incorrect Dosage | p | ||||
| Total | n | % | n | % | ||
| Doctor | 15 | 14 | 93.3 | 1 | 6.7 | |
| Nurse | 96 | 93 | 96.9 | 3 | 3.1 | <10−3 |
| Midwife | 4 | 3 | 75 | 1 | 25 | |
| Orderly | 46 | 30 | 65.2 | 4 | 8.7 | |
| Duration of Treatment in Children | ||||||
| Correct Duration of Treatment | Incorrect Duration of Treatment | p | ||||
| Total | n | % | n | % | ||
| Doctor | 15 | 15 | 100 | 0 | 0 | |
| Nurse | 96 | 96 | 100 | 0 | 0 | 0.00027 |
| Midwife | 4 | 3 | 75 | 1 | 25 | |
| Orderly | 46 | 44 | 95.6 | 2 | 4.3 | |
| Antimalarial Drugs Usually Prescribed to Adults | ||||||
| Correct Dosage | Incorrect Dosage | p | ||||
| Total | n | % | n | % | ||
| Doctor | 15 | 14 | 93.3 | 1 | 6.7 | |
| Nurse | 96 | 85 | 88.5 | 11 | 11.5 | <10−3 |
| Midwife | 4 | 3 | 75 | 1 | 25 | |
| Orderly | 46 | 37 | 80.4 | 9 | 19.6 | |
| Duration of Treatment in Adults | ||||||
| Correct Duration of Treatment | Incorrect Duration of Treatment | p | ||||
| Total | n | % | n | % | ||
| Doctor | 15 | 15 | 100 | 0 | 0 | |
| Nurse | 96 | 87 | 90.6 | 9 | 9.4 | 0.00027 |
| Midwife | 4 | 1 | 75 | 3 | 25 | |
| Orderly | 46 | 43 | 93.5 | 3 | 6.5 | |
| Drug Recommended as First-Line Treatment for Uncomplicated Malaria | ||||||
| ASAQ, AL, or DHA PQ | Others (ACT) | p | ||||
| Total | n | % | n | % | ||
| Doctor | 15 | 15 | 100 | 0 | 0 | |
| Nurse | 98 | 98 | 100 | 0 | 0 | 0.53 |
| Midwife | 4 | 4 | 100 | 0 | 0 | |
| Orderly | 46 | 45 | 97.8 | 1 | 2.2 | |
| Drug Recommended as First-Line Treatment for Complicated Malaria | ||||||
| Artesunate for Injection | Artemether for Injection | p | ||||
| Total | n | % | n | % | ||
| Doctor | 15 | 15 | 100 | 0 | 0 | |
| Nurse | 98 | 96 | 97.9 | 0 | 0 | 0.28 |
| Midwife | 4 | 3 | 75 | 1 | 25 | |
| Orderly | 46 | 44 | 95.6 | 1 | 4.4 | |
Nurses (n = 40/96; 41.7%) and orderlies (n = 25/46; 54.3%) were the most likely to be unaware of NMCP activities. A significant association was found between knowledge of the NMCP activities and professional status (p = 0.00027), as shown in Table 3.
Table 4 shows practitioners’ attitudes in the event of a negative RDT result.
Table 4.
Practitioners’ attitudes in the event of a negative RDT result.
| What to Do in Case of Negative RDT or Microscopy | ||||||
|---|---|---|---|---|---|---|
| Offered Antimalarial Treatment by ACTs | Not Offered Antimalarial Treatment by ACTs | p | ||||
| Total | n | % | n | % | ||
| Doctor | 15 | 11 | 73.3 | 4 | 26.7 | |
| Nurse | 96 | 40 | 41.6 | 56 | 58.4 | <10−3 |
| Midwife | 4 | 2 | 50 | 2 | 50 | |
| Orderly | 46 | 19 | 41.3 | 27 | 58.7 | |
Quite often, we reported mistakes in prescribing antimalarial drugs to adults or children. Specifically, nurses, midwives, and orderlies become used to making mistakes regarding the treatment duration for children.
When discussing known treatments for uncomplicated malaria in children or adults, all the practitioners answered ASAQ, AL, or DHA PQ. According to the survey, 98.1% of the respondents mentioned using Artesunate for injection. AL was the most prescribed treatment for uncomplicated malaria (children or adults).
Most practitioners (89/161; 55.3%) offered antimalarial treatment by ACTs in case of a negative RDT result. This practice was observed with all professional status categories, although the phenomenon was more familiar for the orderlies (58.7%), nurses (58.4%), and midwives (50%) (Table 3).
4. Discussion
ACTs have been highly effective for nearly 20 years, but the emergence of drug-resistant parasites now threatens their efficacy [17,18]. The World Health Organization has advised countries that are affected by malaria to revise their treatment policies due to the possibility of the emergence and expansion of artemisinin-resistant malaria parasites in Southeast Asian countries as well as in other endemic areas [19]. To delay this resistance, applying the control measures recommended by the NMCP for correct management in private nurseries is essential. It is, therefore, important to assess the knowledge and practices of private nurseries since they are sometimes the first point of contact. This information can help guide discussions on the involvement of the private sector in NMCP activities aimed at controlling or even eliminating malaria.
However, low compliance with malaria national protocols by healthcare workers remains a problem in many countries in sub-Saharan Africa [6,20]. As in most African countries [21,22], practitioners’ knowledge about malaria transmission, signs, symptoms, biological tests, antimalarial drugs, and vector control was generally good.
Some clinical manifestations specific to malaria constitute benchmarks for the private nursery to propose antimalarial drugs for curative treatment. These include fever, headache, asthenia, and body aches. Other authors have also described these signs with varying frequencies.
One of the foundations of malaria control is the efficient management of cases at public health facilities. Since 2012, the WHO has advised that clinical diagnoses should be confirmed by parasitological methods [23]. In Côte d’Ivoire, clinical diagnosis was the malaria diagnosis method most used by private or public health centre workers, while confirmation by RDTs was mainly cited and used. The WHO recommends thick and thin blood smears and RDTs for the biological confirmation of suspected malaria cases. In Côte d’Ivoire, RDT testing is the first approach at health facilities such as urban health centres and training hospitals. We resort to microscopy only at the tertiary level [6,11,16].
A Nigerian study reported inadequate evaluation and underreporting of clinical findings, which were more common in private than public health facilities [24]. The same observation was reported in our study and previously in Côte d’Ivoire [6]. Government agencies tend to provide more training support to health providers working in public health facilities compared to those working in private facilities. They may comply more effectively with practice guidelines [6,10]. It seems likely that a higher patient load in public health facilities would make such adherence difficult.
In the past, most patients received malaria treatment without undergoing laboratory confirmation tests. Nowadays, this practice is prohibited. The Côte d’Ivoire National Malaria Treatment Policy Guidelines were recently revised in 2018, making parasitological test confirmation mandatory for diagnosing and treating malaria in all age groups and types of patients [16]. Notably, RDTs were successful in diagnosing a high proportion of patients suffering from malaria.
The frequent use of RDT was possible because it is currently promoted as an acceptable alternative to microscopy, where the latter is not available or feasible [3,14].
The NMCP has implemented it for free in public health facilities but not in private ones. This can be explained by the fact that patients pay for care in the private sector. In addition, there is a clear desire on the part of the private sector not to collaborate with the NMCP in order to avoid supervision. Different authors have demonstrated this problem of adequacy and adherence between a national care policy and the real practice of private pharmacy auxiliaries in Cote d’Ivoire or of health stakeholders in other African countries, such as Kenya and Benin [5,6,13].
It was in 2018 that Cote d’Ivoire’s NMCP introduced new policy guidelines. Still, until this study, reinforcement or follow-up training had yet to be offered to malaria practitioners working at private health centres regarding the national protocols for malaria management. Once again, knowledge regarding malaria case management must be improved in the HRD of Abidjan 1 and 2 through training if the aim is to achieve malaria control. Therefore, we can look at various initiatives implemented in other African countries [25].
Possible reasons for this poor performance include the unavailability of the current malaria treatment protocols and guidelines for reference at private health facilities and the lack of training, mentorship, support, and supervision of malaria case management by the NMCP. Our finding was similar to that of Wanzira et al. (2021): the lack of training among health facility staff significantly contributes to poor performance [26].
This is especially important given that most of the population seeks care from private health facilities [6]. This highlights the need for the NMCP to collaborate with other health departments within the Ministry of Health to improve training for private healthcare facilities, as it currently does for public healthcare facilities. This support should encourage data capture and transmission to the NMCP and the use of data for decision-making.
Usually, the factors that influence health workers’ knowledge of malaria frequently include education and working experience [27]. The comparison of years of working experience reveals that practitioners with fewer years of working experience are more likely to have a solid knowledge of malaria than those with more extensive expertise, because they have received more recent and up-to-date training.
About 87% of children and adults managed in the private nursery had an appropriate treatment regimen for uncomplicated malaria. Wrong dosage prescription was noted in 21 (13.1%) children and 22 (13.6%) adults. The antimalarial prescription was inappropriate in the duration of treatment in 3 (1.8%) children and 15 (9.3%) adults. Incorrect administration of ACTs, particularly insufficient dosages, can not only result in treatment failure but may also cause drug pressure, leading to the eventual emergence of parasite resistance to the medications. Indeed, the reduced efficacy of artemisinins and ACTs has already been reported in some parts of Asia [28]. A study conducted in Nigeria’s Federal Capital Territory (FCT) found that the prescription of artemisinin-based combination therapy (ACT) for uncomplicated malaria was incorrect in 37% of cases [29].
This study consisted of a cross-sectional survey of the Abidjan District, so the main limitation is that the results may only generally apply to some countries. It would be interesting to carry out a more extensive survey in Abidjan and other cities of the Ivory Coast to understand the knowledge and practices of practitioners.
5. Conclusions
Practitioners of private nurseries in the Abidjan 1 and 2 health regional directions had good knowledge of malaria and better practices. However, general knowledge about malaria and the National Malaria Treatment Guidelines could be higher in the private sector. Therefore, it is essential to reinforce practitioners’ understanding and use of the NMCP to improve malaria case management and disease control in these two regions. Private nurseries should be encouraged and supported to consider TDR or microscopy results.
Author Contributions
K.E.G.M., K.-B.P.C.M., K.-T.A. and K.K.F. contributed to the study design and analyzed the research data. G.N.K.A., A.K.E., B.-T.A.V., M.A.J.S. and D.V. provided additional articles related to the topic. Y.W. and M.E.I.H. wrote the review, which was then read and approved by all other authors. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any specific funding from funding agencies.
Acknowledgments
We would like to gratefully thank all the staff of Health Care Facilities and Professions (HCFP), the private nurseries, and the Diagnosis and Research Centre on AIDS and Other Infectious Diseases, Abidjan, Ivory Coast.
Conflicts of Interest
The authors do not declare any conflicts of interest. This study was approved by the Department of Health Care Facilities and Professions (HCFP) of Côte d’Ivoire. Oral consent was obtained prior to the initiation of the investigation.
References
- WHO. World Malaria Report 2022; World Health Organization: Geneva, Switzerland, 2023. [Google Scholar]
- Ministry of Health and Control of Ivory Coast. National Malaria Control Programme 2021: National Strategic Plan for Malaria Control 2016–2021; ‘National strategic advocacy plan for the fight against malaria in Côte d’Ivoire (PSNPP) 2021–2025’; Ministry of Health and Control of Ivory Coast: Abidjan, Côte d’Ivoire, 2016. [Google Scholar]
- World Health Organization. Guidelines for the Treatment of Malaria; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- World Health Organization. Guidelines for the Treatment of Malaria; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Amboko, B.; Stepniewska, K.; Malla, L.; Machini, B.; Bejon, P.; Snow, R.W.; Zurovac, D. Determinants of improvement trends in health workers’ compliance with outpatient malaria casemanagement guidelines at health facilities with available “test and treat” commodities in Kenya. PLoS ONE 2011, 16, e0259020. [Google Scholar]
- Bedia-Tanoh, V.A.; Angora, É.K.; Miezan, S.A.J.; Koné-Bravo, E.D.M.; Konaté-Touré, A.; Bosson-Vanga, H.; Kassi, F.K.; Kiki-Barro, P.C.M.; Djohan, V.; Menan, H.E.I.; Yavo, W. Knowledge and practices of private pharmacy auxiliaries on malaria in Abidjan, Côte d’Ivoire. Malar. J. 2023, 22, 330. [Google Scholar] [CrossRef]
- Plucinski, M.M.; Ferreira, M.; Ferreira, C.M.; Burns, J.; Gaparayi, P.; Joao, L.; Da Costa, O.; Gill, P.; Samutondo, C.; Quivinja, J.; et al. Evaluating malaria case management at public health facilities in two provinces in Angola. Malar. J. 2017, 16, 186. [Google Scholar] [CrossRef]
- Plucinski, M.M.; Guilavogui, T.; Camara, A.; Ndiop, M.; Cisse, M.; Painter, J.; Thwing, J. How far are we from reaching universal malaria testing of all fever cases? Am. J. Trop. Med. Hyg. 2018, 99, 670–679. [Google Scholar] [CrossRef] [PubMed]
- O’Boyle, S.; Bruxvoort, K.J.; Ansah, E.K.; Burchett, H.E.D.; Chandler, C.I.R.; Clarke, S.E.; Goodman, C.; Mbacham, W.; Mbonye, A.K.; Onwujekwe, O.E.; et al. Patients with positive malaria tests not given artemisinin-based combination therapies: a research synthesis describing under-prescription of antimalarial medicines in Africa. BMC Med. 2020, 18, 17. [Google Scholar] [CrossRef] [PubMed]
- Kabaghe, A.N.; Visser, B.J.; Spijker, R.; Phiri, K.S.; Grobusch, M.P.; Van, V.M. Health workers’ compliance to rapid diagnostic tests (RDTs) to guide malaria treatment: a systematic review and meta-analysis. Malar. J. 2016, 15, 163. [Google Scholar] [CrossRef] [PubMed]
- Fulgence, K.K.; Massafoma, K.E.G.; Sebastien, M.A.J.; Alain, G.N.K.; Akoua, V.B.; Etienne, A.K.; Abibatou, K.; Henriette, V.A.; Marie, K.P.C.; Vincent, D.; et al. Evaluation of Malaria Microscopy Diagnostic Performance at 40 Public Health Facilities in Abidjan, Côte d’Ivoire in 2020. Acta Parasitol. 2024, 11, 16. [Google Scholar] [CrossRef] [PubMed]
- Steinhardt, L.C.; Chinkhumba, J.; Wolkon, A.; Luka, M.; Luhanga, M.; Sande, J.; Oyugi, J.; Ali, D.; Mathanga, D.; Skarbinski, J. Quality of malaria case management in Malawi: results from a nationally representative health facility survey. PLoS ONE 2014, 9, e89050. [Google Scholar] [CrossRef] [PubMed]
- Ganfon, H.; Ekanmian, G.; Amoussou, L.; Daniel-Garcia, E.; Allabi, A.C. Evaluation of the knowledge and attitude of pharmacists about the national malaria control policy in southern Benin. Malar. J. 2017, 16, 231. [Google Scholar] [CrossRef]
- Kalilani-Phiri, L.V.; Lungu, D.; Coghlan, R. Knowledge and Malaria treatment practices using artemisinin combination therapy (ACT) in Malawi: survey of health professionals. Malar. J. 2011, 10, 279. [Google Scholar] [CrossRef] [PubMed]
- Miezan, A.J.S.; Gnagne, A.P.; Bedia-Tanoh, A.V.; Kone, E.G.M.; Konate-Toure, A.A.; Angora, K.E.; Bosson-Vanga, A.H.; Kassi, K.F.; Kiki-Barro, P.C.M.; Djohan, V.; et al. Molecular epidemiology of non-falciparum Plasmodium infections in three different areas of the Ivory Coast. Malar. J. 2023, 22, 211, PMCID:PMC10357878. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Control of Ivory Coast. Order no. n°0190/CAB/MSHPCMU of November 27, 2018 redefning the therapeutic and preventive regimen for malaria in Ivory Coast; Ministry of Health and Control of Ivory Coast: Abidjan, Côte d’Ivoire, 2018. [Google Scholar]
- Phyo, A.P.; Nkhoma, S.; Stepniewska, K.; Ashley, E.A.; Nair, S.; McGready, R.; ler Moo, C.; Al-Saai, S.; Dondorp, A.M.; Lwin, K.M.; et al. Emergence of artemisinin-resistant malaria on the western border of Thailand: a longitudinal study. Lancet 2012, 379, 1960–1966. [Google Scholar] [CrossRef] [PubMed]
- Toure, O.A.; Assi, S.B.; Kiki-Barro, P.M.C.; Yavo, W.; Abba, T.; Tiacoh, L.N.; Konate, A.A.; Angora, E.K.; Bedia, V.A.; Menan, H.; et al. Efficacy and safety of artesuante-amodiaquine and artemether lumefantrine, the first line malaria treatment in six sentinel’s sites of Côte d’Ivoire, West Africa. Ann. Parasitol. 2020, 66, 561–571. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Methods for Surveillance of Antimalarial Drug Efficacy; Global Malaria Programme, WHO: Geneva, Switzerland, 2009. [Google Scholar]
- Namuyinga, R.J.; Mwandama, D.; Moyo, D.; Gumbo, A.; Troell, P.; Kobayashi, M.; Shah, M.; Bauleni, A.; Vanden, E.J.; Rowe, A.K.; et al. Health worker adherence to malaria treatment guidelines at outpatient health facilities in Southern Malawi following implementation of universal access to diagnostic testing. Malar. J. 2017, 16, 40. [Google Scholar] [CrossRef]
- Blanco, M.; Suárez-Sanchez, P.; García, B.; Nzang, J.; Ncogo, P.; Riloha, M.; Berzosa, P.; Benito, A.; Romay-Barja, M. Knowledge and practices regarding malaria and the National Treatment Guidelines among public health workers in Equatorial Guinea. Malar. J. 2021, 20, 21, PMCID:PMC7789308. [Google Scholar] [CrossRef] [PubMed]
- Asante, K.P.; Abokyi, L.; Zandoh, C.; Owusu, R.; Awini, E.; Sulemana, A.; Amenga-Etego, S.; Adda, R.; Boahen, O.; Segbaya, S.; et al. Community perceptions of malaria and malaria treatment behaviour in a rural district of Ghana: implications for artemisinin combination therapy. BMC Public Health 2010, 10, 409. [Google Scholar] [CrossRef]
- Nankabirwa, J.; Brooker, S.J.; Clarke, S.E.; Fernando, D.; Gitonga, C.W.; Schellenberg, D.; Greenwood, B. Malaria in school-age children in Africa: an increasingly important challenge. Trop. Med. Int. Health 2014, 19, 1294–1309. [Google Scholar] [CrossRef]
- Gbotosho, G.O.; Happi, C.T.; Ganiyu, A.; Ogundahunsi, O.A.; Sowunmi, A.; Oduola, A.M. Potential contribution of prescription practices to the emergence and spread of chloroquine resistance in south-west Nigeria: caution in the use of artemisinin combination therapy. Malar. J. 2009, 8, 313, PMCID:PMC2807872. [Google Scholar] [CrossRef] [PubMed]
- Juma, E.; Zurovac, D. Changes in health workers’ malaria diagnosis and treatment practices in Kenya. Malar. J. 2011, 10, 1. [Google Scholar] [CrossRef]
- Wanzira, H.; Tumwine, D.; Bukoma, P.; Musiime, A.; Biculu, J.; Ediamu, T. An assessment of the knowledge, practices and resources during the delivery of malaria health care services among private health care practitioners: a cross section study in the Mid-Western Region of Uganda. BMC Health Serv. Res. 2021, 21, 788, PMCID:PMC8356442. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Tang, S.; Yang, J.; Shao, T.; Shao, O.; Liu, C.; Feng, D.; Fu, H.; Chen, X.; Hu, T.; et al. Improving local health workers’ knowledge of malaria in the elimination phase-determinants and strategies: a cross-sectional study in rural China. Malar. J. 2017, 16, 210. [Google Scholar] [CrossRef] [PubMed]
- Lim, P.; Alker, A.P.; Khim, N.; Shah, N.K.; Incardona, S.; Doung, S.; Yi, P.; Bouth, D.M.; Bouchier, C.; Puijalon, O.M.; et al. Pfmdr1 copy number and arteminisin derivatives combination therapy failure in falciparum malaria in Cambodia. Malar. J. 2009, 8, 11. [Google Scholar] [CrossRef] [PubMed]
- Udoh, E.; Oyo-Ita, A.; Odey, F.; Effa, E.; Esu, E.; Oduwole, O.; Chibuzor, M.; Meremikwu, M. Management of uncomplicated malaria in underfives in private and public health facilities in South-eastern Nigeria: a clinical audit of current practices. Malar. Res. Treat. 2013, 2013, 575080, PMCID:PMC3564278. [Google Scholar] [CrossRef] [PubMed]
© 2025 Copyright by Authors. Licensed as an open access article using a CC BY 4.0 license.