Afr. J. Parasitol. Mycol. Entomol. , 3(1), 5; doi:10.35995/ajpme03010005
Article
The Prevalence of Anemia and Associated Infections Among Children Under 5 Years of Age in the Senegal River Valley, Mauritania
1
Faculty of Medicine, University of Nouakchott, Nouakchott BP 880, Mauritania; bezeidmohamedine@yahoo.fr (O.M.); salkamohamed94@yahoo.fr (S.M.M.)
2
Mauritania Endemic Diseases Control Initiative “MEDCINGO”, Nouakchott BP 8401, Mauritania; mhabdou4@gmail.com
3
Genomes and Environments Research Unit (GeMi), Department of Biology, Faculty of Science and Technology, University of Nouakchott, Nouakchott BP 880, Mauritania; firstname.lastname@email.com
*
Corresponding author: hmoukah2002@yahoo.fr; Tel.: +222-2204-7283
†
These authors contributed equally to this work.
How to Cite: Mohamedine, O.; Mohamed, S.M.; Mohamed, A.; Moukah, M.O. The Prevalence of Anemia and Associated Infections Among Children Under 5 Years of Age in the Senegal River Valley, Mauritania. Afr. J. Parasitol. Mycol. Entomol., 2025, 3(1): 5; doi:10.35995/ajpme03010005.
Received: 1 March 2025 / Accepted: 13 October 2025 / Published: 13 December 2025
Abstract
:Background: Anemia, malaria, and intestinal parasitic infection pose significant health threats to children in developing countries, adversely affecting their cognitive development and nutritional status and increasing their susceptibility to other infectious diseases. In Mauritania, the high prevalence of anemia, particularly in rural areas, along the Senegal River is alarmingly high and remains a critical public health concern. Methods: A descriptive cross-sectional study was conducted between August and October 2022 in six health facilities along the Mauritanian side of the Senegal River. Anemia was defined according to WHO criteria, and hemoglobin levels were measured using a HemoCue® Hb 301 analyzer. Pinworm (Enterobius vermicularis) infection was diagnosed using the adhesive tape (Scotch tape test) method. Malaria was diagnosed via thick blood smears stained with 10% Giemsa and examined under a microscope. Although thin smears were not performed due to resource limitations, Plasmodium falciparum was identified based on its distinctive morphological features observed in thick smears. Results: Anemia was detected in 75.1% of the 361 children enrolled, with a mean hemoglobin level of 7.3 g/dL. The highest prevalence (90%) was found among children aged 6 to 24 months. Pinworm infection was observed in 20.3% of participants, while malaria showed a low overall prevalence of 2.9%, with all cases confined to the upper valley and attributed to P. falciparum. Conclusion: This study highlights a high burden of anemia among children aged 6 to 59 months on the Mauritanian side of the Senegal River basin. The co-occurrence of intestinal parasitic infections and malaria, though limited, further emphasizes the need for integrated control strategies, including nutritional support and preventive deworming.
Keywords:
anemia; Oxyuriasis; malaria; prevalence in children under five; Senegal River; Mauritania1. Introduction
According to the World Health Organization (WHO), anemia, malaria, and intestinal parasitic infections remain major public health challenges in many developing countries [1]. The complex interplay between these conditions has attracted increasing attention, particularly in children under five years of age, who represent one of the most vulnerable population groups [2]. Anemia most often results from deficiencies in essential micronutrients, such as iron, folic acid, and vitamin B12, either in isolation or in combination [3,4]. In addition, chronic inflammation and infections, especially parasitic diseases, can exacerbate anemia by impairing nutrient absorption, increasing nutrient losses, and affecting red blood cell production [5]. These conditions can hinder physical growth, delay cognitive development, and compromise both digestive and immune system functions in early childhood.
In Mauritania, the most recent Demographic and Health Survey (EDSM, 2021) reported a prevalence of anemia of 77% among children aged 6 to 59 months, with rates exceeding 82% in rural areas [6]. Malaria remains one of the leading causes of morbidity, accounting for more than 18% of outpatient consultations nationwide [7], and its contribution to anemia is well documented through mechanisms involving hemolysis and bone marrow suppression. Enterobius vermicularis (pinworm) infection, although often perceived as benign, has been associated with diarrhea, anemia, growth retardation, and weight loss in children [8,9,10]. Its true morbidity burden is likely underestimated due to diagnostic limitations, as routine stool examinations have low sensitivity compared to that of the Scotch tape test, which is more effective for detecting eggs [11].
Despite the recognized impact of these conditions, there is a paucity of integrated epidemiological data examining their co-occurrence in Mauritania, particularly in the Senegal River basin. This region is characterized by ecological heterogeneity, seasonal malaria transmission, variable access to healthcare, and socio-economic conditions that may favor persistent parasitic infections and nutritional deficiencies. Most previous studies have focused on single diseases in isolation, thereby underestimating their combined effect on child health. Generating updated, location-specific data on the prevalence and distribution of anemia, malaria, and E. vermicularis infection is essential for designing cost-effective, multi-disease control strategies.
The aim of this study was therefore to assess the prevalence of anemia, malaria, and E. vermicularis infection among children aged 6 to 59 months in the Senegal River basin of Mauritania, a setting where environmental, socio-economic, and healthcare access factors may interact to amplify disease burden.
2. Methods
2.1. Study Sites
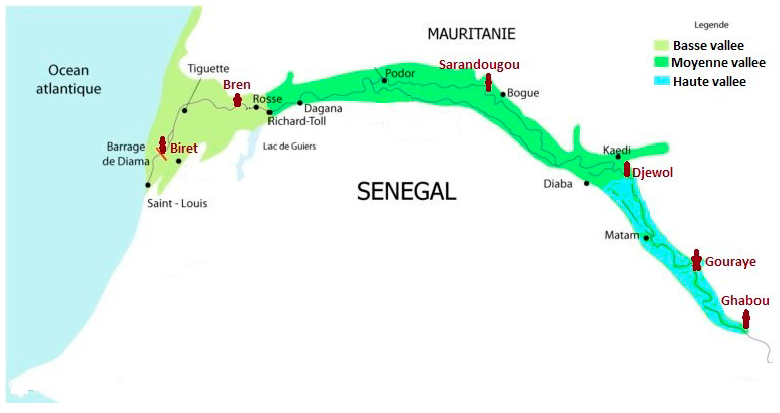
This cross-sectional, descriptive study was carried out from August to October 2022 in six healthcare facilities along the Senegal River basin in Mauritania. The selected sites spanned three biogeographic zones: Biret and Breun in the lower valley, Sarandougou and Djewol in the middle valley, and Gouraye and Ghabou in the upper valley (Figure 1). These localizations were chosen for their ecological relevance and the availability of functional health services.
Figure 1.
The location of the localities surveyed along the Senegal River basin in Mauritania, 2022.
Figure 1.
The location of the localities surveyed along the Senegal River basin in Mauritania, 2022.
2.2. Data Collection
Data were collected using a standardized medical form that included the child’s age, sex, reason for consultation, clinical symptoms, body temperature, presumptive diagnostics, and laboratory results.
2.3. Inclusion and Exclusion Criteria
All children aged 6 to 59 months presenting to the health facilities who had undergone both blood sampling and the Scotch tape test were eligible for inclusion, with informed consent provided by their parents or guardians. To avoid potential bias in hemoglobin measurements, we excluded children who had received a blood transfusion within 120 days prior to the data collection.
2.4. Laboratory Analysis
Hemoglobin levels were measured using the HemoCue® Hb 301 analyzer, with anemia defined as a hemoglobin level below 11 g/dL, following WHO guidelines [2]. The adhesive tape test (also known as the Scotch tape test) was used to detect Enterobius vermicularis eggs, applied around the anal area in the early morning before defection. Malaria diagnosis was made using a thick blood smear (TBS). The identification of Plasmodium falciparum in blood smears was based on specific morphological characteristics such as multiple ring forms within the erythrocytes and crescent-shaped gametocytes. Children exhibiting symptoms such as a cough, rapid breathing, rales, or signs of lung consolidation were diagnosed with bronchopneumonia.
2.5. Statistical Analysis
Data were entered into Microsoft Excel and analyzed using EpiInfo™ 7.2.2. Categorical variables were compared using the Chi-square test, while continuous variables were analyzed using an ANOVA. A 95% confidence interval was used for all statistical tests, with p-values below 0.05 considered statistically significant.
2.6. Ethical Considerations
The study protocol was approved by the relevant ethical authority. Informed consent was obtained from all parents or guardians prior to participation. Children diagnosed with anemia, malaria, or parasitic infections received free treatment, including iron supplementation, antimalarial medication, and anti-parasitic therapy.
3. Results
3.1. Study Population
Among the 539 children aged 6 to 59 months who presented at the six participating health facilities, 361 met the inclusion criteria and were enrolled in the study. Males accounted for 53.5% of the participants, yielding a sex ratio of 1.15.
3.2. Prevalence and Severity of Anemia
Anemia (hemoglobin <11 g/dL) was observed in 271 children, corresponding to a prevalence of 75.1%. The mean hemoglobin concentration among anemic children was 7.3 ± 1.1 g/dL, with values ranging from 5.3 to 10.9 g/dL. Moderate anemia was most common (46.8%), followed by mild anemia (25.5%) and severe anemia (2.8%). The average age of anemic boys was 22.8 ± 2.6 months, and that of girls was 23.2 ± 2.8 months (p = 0.23). Anemia was significantly more prevalent among children aged 6 to 24 months (p = 0.02) (Table 1).
Table 1.
The prevalence and degree of severity of anemia in children aged 6–59 months, by age group, on the right bank of the Senegal River, Mauritania, 2022.
Table 1.
The prevalence and degree of severity of anemia in children aged 6–59 months, by age group, on the right bank of the Senegal River, Mauritania, 2022.
| Degree of Severity | Examined | Age Groupe | p-Value | ||
|---|---|---|---|---|---|
| N = 361 | 6–24 Months N = 131 | 25–36 Months N = 127 | 37–59 Months N = 103 | ||
| moderate Anemia | 169(46.8%) | 64(37.9%) | 59(34.9%) | 46(27.2%) | 0.044 |
| mild Anemia | 92(25.5%) | 47(51.1%) * | 23(25.0%) | 22(23.9%) | 0.019 |
| severe Anemia | 10(2.8%) | 7(70.0%) * | 2(20.0%) | 1(10.0%) | 0.0002 |
| Total | 271(75.1 %) | 118(90.1%) * | 84(66.1%) | 69(67.0%) | 0.000013 |
Note: An asterisk (*) indicates statistically significant differences between age groups. N = number of participants; % = percentage.
3.3. Prevalence by Biogeographic Zone
The upper valley exhibited the highest prevalence of anemia (93.2%) and pinworm infection (20.3%), and it was the only region where malaria cases were reported (Table 2).
Table 2.
The prevalence (%) of anemia, pinworms, and malaria in children aged 6–59 months, by biogeographic zone, on the right bank of the Senegal River, Mauritania, 2022.
Table 2.
The prevalence (%) of anemia, pinworms, and malaria in children aged 6–59 months, by biogeographic zone, on the right bank of the Senegal River, Mauritania, 2022.
| Biogeographic Zone | Prevalence | 95% CI | |||
|---|---|---|---|---|---|
| Examined (N) | Anemia (%) | Pinworm Infection (%) | Malaria (%) | ||
| Lower valley | 129 | 78 (60.5%) | 10 (7.8) | 00 (0.0%) | (8.7–37.9) |
| Middle valley | 115 | 84 (73.0%) | 16 (13.7%) | 00 (0.0%) | (5.2–17.2) |
| High valley | 117 | 109 (93.2%) * | 23 (20.3%) * | 10 (8.5%) * | (10.4–43.2) |
| Total | 361 | 271 (75.1%) | 49 (13.6%) | 10 (2.9%) | |
* Statistically significant differences observed at p < 0.05.
3.4. Clinical and Etiological Presentation
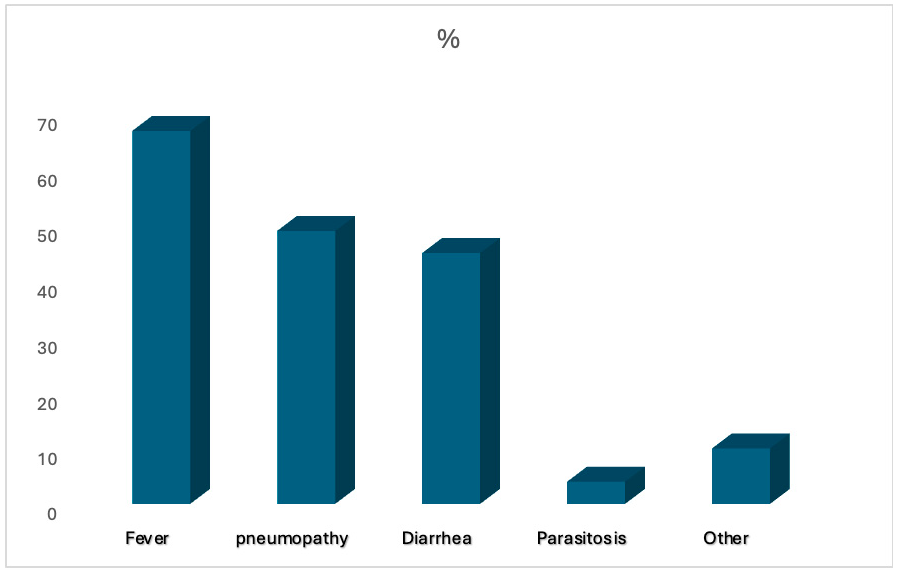
The primary presenting symptom among anemic children was fever, with common clinical signs including pallor, asthenia, tachycardia, and dyspnea. Enterobius vermicularis infections presented with anal pruritus, abdominal pain, diarrhea, and vomiting. Malaria infections were characterized by fever and headache (Figure 2).
Figure 2.
Reasons for consultation among children aged 6–59 months, found in consultation, from the right bank of the Senegal River, Mauritania, 2022.
Figure 2.
Reasons for consultation among children aged 6–59 months, found in consultation, from the right bank of the Senegal River, Mauritania, 2022.
4. Discussion
This study reveals an alarmingly high burden of anemia among children under five years of age in the Senegal River Valley of Mauritania. With a prevalence of 75.1%, the magnitude of this problem far exceeds the WHO threshold of 40%, which defines anemia as a severe public health problem [3,4]. The mean hemoglobin concentration (7.3 g/dL) is comparable to findings from Cameroon (7.4 g/dL) among anemic children aged 6–14 months [12]. Although our study targeted sick children, who are likely at a higher risk of anemia, our results are consistent with the 2021 EDSM survey, which reported a 77% prevalence of anemia among non-hospitalized children in the same age group [6].
Children aged 6–24 months were disproportionately affected, with an anemia prevalence of 90.1% (p = 0.000013). This finding aligns with the existing literature highlighting the vulnerability of this age group due to rapid physiological growth, elevated micronutrient requirements, and increased susceptibility to infections [13]. Severe anemia was particularly common in this age range, underscoring the urgent need for early iron supplementation and targeted nutritional interventions.
Marked disparities were observed across biogeographic zones. The upper valley, characterized by limited healthcare access and environmental conditions favorable to parasitic transmission, recorded the highest rates of anemia (93%) and pinworm infection (20.3%) and all malaria cases. These observations are consistent with previous studies in the Sahel linking poor sanitation, poverty, and inadequate health services to a higher anemia burden [14].
Enterobius vermicularis infection was diagnosed in 13.6% of all children, with the highest prevalence in the upper valley (20.3%, p < 0.05). Pinworm infections can impair iron absorption and contribute to malnutrition and anemia [15]. Malaria prevalence was low (2.9%), consistent with historically low transmission in the Senegal River basin [16]. However, all confirmed malaria cases were due to Plasmodium falciparum, identified morphologically in thick blood smears, and were confined to the upper valley [17]. This species is known to exacerbate anemia through hemolysis and the suppression of erythropoiesis [18].
Most consultations were for fever, respiratory infections, or gastrointestinal complaints, along with asthenia, patterns that mirror national disease surveillance data [7]. Given the non-specific nature of these symptoms, routine hemoglobin screening and regular deworming campaigns should be prioritized in high-risk pediatric populations [19].
Study Limitations
This study is subject to certain limitations, including the data being collected in health facilities, while selection bias may limit generalizability. Despite these limitations, the findings provide a strong rationale for integrated interventions targeting nutrition, sanitation, and parasite control.
5. Conclusions
Anemia and parasitic infections remain major public health concerns among children under five living on the right bank of the Senegal River in Mauritania. Although malaria prevalence was relatively low (2.9%), Plasmodium falciparum was detected in the upper valley, where it likely exacerbates the anemia burden through hemolysis and impaired erythropoiesis. These findings underscore the urgent need for integrated, multisectoral interventions that combine routine iron supplementation, large-scale deworming with Albendazole, improved nutritional support, and strengthened access to primary healthcare. Such coordinated efforts are essential to reducing the high anemia prevalence and its long-term consequences for child growth, development, and survival.
Author Contributions
O.M.: Medical aspects, supervision, and manuscript corrections. S.M.M.: Medical aspects, supervision, and manuscript corrections. A.M.: Biological aspects and manuscript corrections. M.O.M: Design, supervision, data acquisition, and manuscript writing. All of the authors have read and approved the final version of the manuscript.
Funding
The survey was conducted with the financial and logistical support of the Mauritanian Initiative for the Fight against Endemic Diseases (MEDCINGO), Nouakchott Mauritania, BP: 8401.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Before enrolment, the objectives of this study were fully explained to the participants, and informed consent was obtained from adult patients or/legal guardians of children. Only individual patients or legal guardians who signed (or fingerprinted) the consent form participated in this study.
Consent for Publication
Not applicable.
Acknowledgments
We thank Dieye Mamadou, senior biology technician at the Rosso Health Center, Regional Health Directorate (DRAS) of Trarza, and Elhadj DEM, a biologist at Boghé Hospital, Regional Health Directorate (DRAS) of Brakna, for their field contributions. We also acknowledge Mohamedin Ahmedou and MedAbdallahi MedLemine for their contributions to the statistical data analysis.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- OMS/UNICEF. Joint statement: Focusing on Anaemia, Towards an Integrated Approach for Effective Anaemia Control; Joint Statement by World Health Organization and the United Nations Children’s Fund; WHO: Geneva, Switzerland, 2004. [Google Scholar]
- Stephenson, L.S.; Latham, M.C.; Ottesen, E.A. Malnutrition and parasitic helminth infections. Parasitology 2000, 121, S23–S38. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Anaemia Prevalence and Number of Individuals Affected; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Levy, A.; Fraser, D.; Rosen, S.D.; Dagan, R.; Deckelbaum, R.J.; Coles, C.; Naggan, L. Anaemia as a risk factor for infectious diseases in infants and toddlers: Results from a prospective study. Eur. J. Epidemiol. 2010, 20, 277–284. [Google Scholar] [CrossRef]
- Institut National de la Statistique(INS). Enquête Démographique et de Santé 2021 (EDSM); Ministère de la Santé: Nouakchott, Mauritania, 2022. Available online: https://ansade.mr/fr/enquete-demographique-et-de-sante-de-la-mauritanie-edsm-2019-2021 (accessed on 9 April 2024).
- Plan National de Développement Sanitaire(PNDS); 2022–2030 V.I, Min Santé Mauritanie. Available online: https://p4h.world/app/uploads/2024/10/PNDS-2022-2030-Volume1_Mauritanie.x23411.pdf (accessed on 9 April 2024).
- Bourée, P. Les parasitoses intestinales sont encore fréquentes. Médecine et Santé Tropicales 2015, 25. [Google Scholar] [CrossRef]
- Urbani, C.; Toure, A.; Hamed, O.A.; Albonico, M.; Kane, I.; Cheikna, D.; Hamed, N.O.; Montresor, A. Intestinal parasitic infection and schistosomiasis in the Senegal River valley of the Islamic Republic of Mauritania. Med. Trop. 1997, 57, 157–160. [Google Scholar]
- Ouldbezeid, M.; Garba, A. Mbaye A et Konaté Parasitoses intestinales et schistosomiases chez les écoliers de la rive Mauritanienne du fleuve Sénégal. Annales Africaine de Médecine 2010, 3, 657–573. [Google Scholar]
- Dudlová, A.; Juriš, P.; Jarčuška, P.; Vasilková, Z.; Vargová, V.; Sumková, M.; Krčméry, V. The Incidence of Pinworm (Enterobius Vermicularis) in Pre-school and School Aged Children in the Eastern Slovakia. Helminthologia 2018, 55, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Tietche, F.; Njiki, D.; Tetanye, E. Facteurs épidémiologiques associés aux anémies sévères de l’enfant consultant en urgence à l’hôpital Central de Yaoundé (Cameroun). Bull. Liais. Doc. OCEAC 1993, 26, 50–59. [Google Scholar]
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; de Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J.; Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef] [PubMed]
- Balarajan, Y.; Ramakrishnan, U.; Ozaltin, E.; Shankar, A.H.; Subramanian, S.V. Anaemia in low-income and middle-income countries. Lancet 2011, 378, 2123–2135. [Google Scholar] [CrossRef] [PubMed]
- Faye, O.; Ndir, O.; Gaye, O.; Dieng, T.; Dieng, Y.; Bah, I.B.; Diallo, S. Étude de la prévalence du paludisme dans le bassin du fleuve Sénégal en 1991. Dakar Médical 1997, 42, 83–86. [Google Scholar]
- Ouldabdallahi, M; Ouldbezeid, M.; Lemrabot, M.A.; Ouldelvally, A.; Ouldkhairi, M.L.; Dialw, B.; Basco, L. Study of morbidity and Plasmodium species in the several geographic-climatic areas of Mauritania. Bull. Soc. Pathol. Exot. 2015, 108, 112–116. [Google Scholar] [CrossRef] [PubMed]
- Moukah, M.O.; Ba, O.; Ba, H.; LemineOuldKhairy, M.; Faye, O.; Bogreau, H.; Simard, F.; Basco, L.K. Malaria in three epidemiological strata in Mauritania. Malar. J. 2016, 15, 204. [Google Scholar] [CrossRef] [PubMed]
- Ouldabdallahi, ·M.; Ouldbezeid, M.; Dieye, B.; Yacine, O. Faye. Study of the incidence of malaria in febrile patients and among schoolchildren in the region of Trarza, Islamic Republic of Mauritania. Bull. Soc. Pathol. Exot. 2011, 104, 288–290. [Google Scholar] [CrossRef] [PubMed]
- Price, R.N.; Simpson, J.A.; Nosten, F.; Luxemburger, C.; Hkirjaroen, L.; Kuile, F.T.; Chongsuphajaisiddhi, T.; White, N.J. Factors contributing to anemia after uncomplicated falciparum malaria. Am. J. Trop. Med. Hyg. 2001, 65, 614–622. [Google Scholar] [CrossRef] [PubMed]
- WHO. Preventive chemotherapy to control soil-transmitted helminth infections in at-risk population groups. Available online: https://www.who.int/publications/i/item/9789241550116 (accessed on 9 April 2024).
© 2025 Copyright by Authors. Licensed as an open access article using a CC BY 4.0 license.